ABOUT
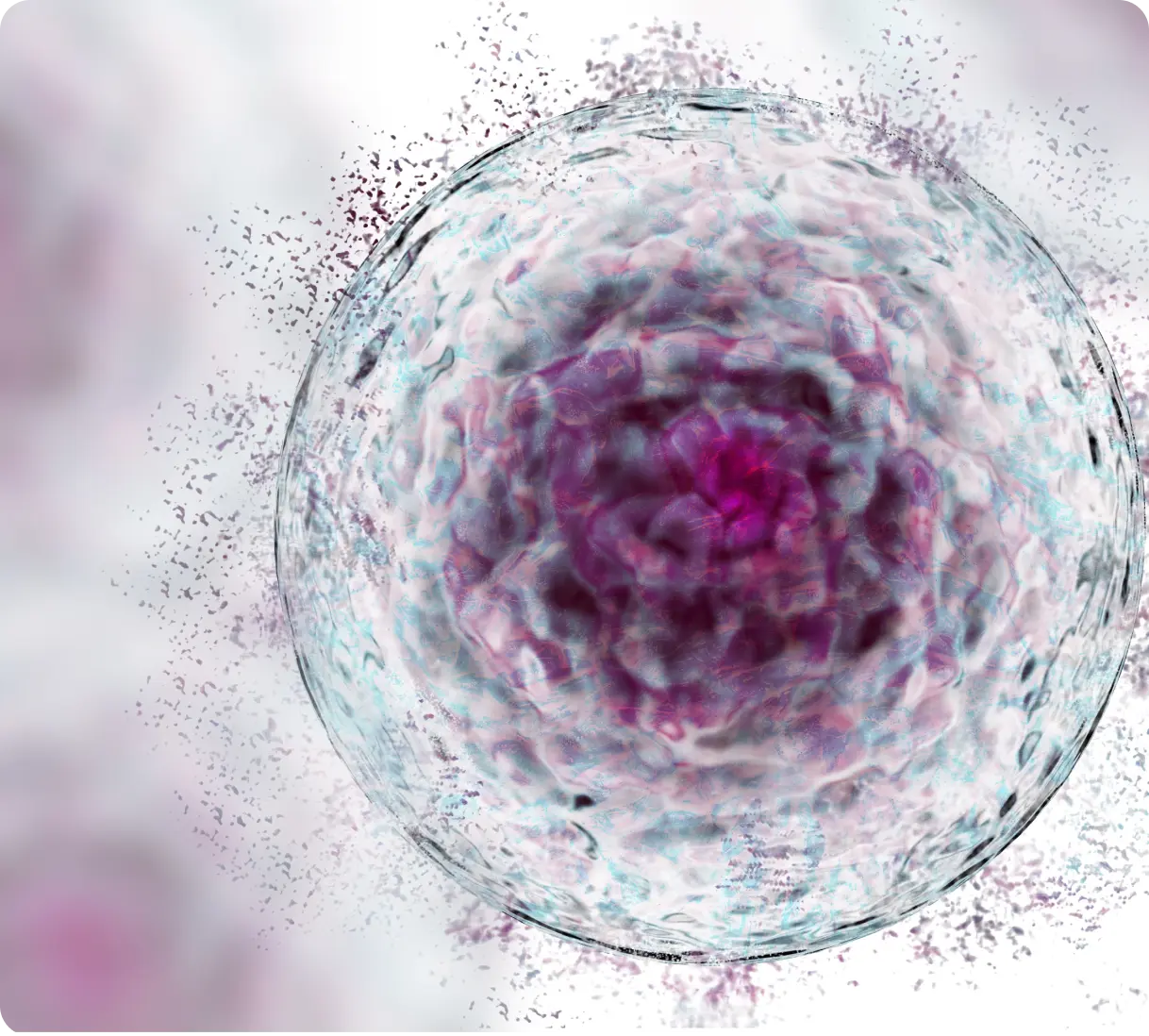
Cell Death:
See, Interpret, Target, Amplify
MISSION
Improve how clinicians see, interpret, target and even amplify cell death to evaluate, personalise and adapt patient care in real-time.
VISION
To unlock the insights from and harness the potential of treatments targeting and amplifying cell death.
Cell death is a fundamental biological process that plays a crucial role in maintaining the health and proper functioning of our bodies.
Cell death can be induced by external factors like burning, freezing, physical trauma and poison, but it is also a critical process to ensure unwanted, damaged or infected cells are eliminated, and for proper development, growth, and repair of tissues.
Cell death is essential in many processes in our bodies, for example:
When our cells are deprived of oxygen and nutrients (e.g. after a heart attack or stroke) they die and are cleared away.
Regulating our immune system, deleting self-reactive immune cells in newborns as their immune system develops so preventing autoimmune diseases.
In embryonic development, cell death eliminates excessive cells like the webbing between fingers.
Tumour suppression, by preventing the uncontrolled growth of abnormal cells.
There are various tightly controlled mechanisms which govern how and when cells die. Disruption of this regulation can contribute to the development of various diseases, including:
Neurodegenerative disease and autoimmune disorders: can result from excessive cell death
Cancer: can develop when there is insufficient (too little) cell death and abnormal cells accumulate rather than being eliminated
Imagine being able to visualise, target and even amplify cell death in real time.
Understanding cell death opens new avenues to treat injury and disease.
Predicting and monitoring response to treatment is an essential function of oncologic imaging* but current approaches fall short.
There is an urgent need for fast and reliable methods that assess therapeutic efficacy, safety and toxicity in real time.
Such an approach would enable the choice of therapy and dose to be optimised for the individual patient in real-time, minimising side effects and avoiding time and money spent on drugs that don’t work, or unnecessary additional procedures.
Patients want more understanding of how they will respond to therapy.
The holy grail of cancer treatment is truly personalised care; a treatment strategy for the patient that is personalised to them and adapts based on their cancer’s response. For a patient, the important question is: “Is my therapy going to work? Is my therapy working?”
Current monitoring of therapeutic results is over weeks and months.
In current clinical practice, care teams evaluate response to therapy (the death of cancer cells) using indirect methods which measure changes in tumour size, growth and metabolism over weeks and months following treatment initiation, rather than measuring cell death directly in real time outcomes.
* Nishino M,Hatabu H, Hodi FS. Imaging of cancer immunotherapy: current approaches and future directions. Radiology 2019; 290:9–22
Amplificare has developed a novel pan-cancer tool that specifically identifies dead and dying cells.
